Abstract
Food insecurity (FI) and water insecurity (WI) are linked with HIV vulnerabilities, yet how these resource insecurities shape HIV prevention needs is understudied. We assessed associations between FI and WI and HIV vulnerabilities among urban refugee youth aged 16–24 in Kampala, Uganda through individual in-depth interviews (IDI) (n = 24), focus groups (n = 4), and a cross-sectional survey (n = 340) with refugee youth, and IDI with key informants (n = 15). Quantitative data was analysed via multivariable logistic and linear regression to assess associations between FI and WI with: reduced pandemic sexual and reproductive health (SRH) access; past 3-month transactional sex (TS); unplanned pandemic pregnancy; condom self-efficacy; and sexual relationship power (SRP). We applied thematic analytic approaches to qualitative data. Among survey participants, FI and WI were commonplace (65% and 47%, respectively) and significantly associated with: reduced SRH access (WI: adjusted odds ratio [aOR]: 1.92, 95% confidence interval [CI]: 1.19–3.08; FI: aOR: 2.31. 95%CI: 1.36–3.93), unplanned pregnancy (WI: aOR: 2.77, 95%CI: 1.24–6.17; FI: aOR: 2.62, 95%CI: 1.03–6.66), and TS (WI: aOR: 3.09, 95%CI: 1.22–7.89; FI: aOR: 3.51, 95%CI: 1.15–10.73). WI participants reported lower condom self-efficacy (adjusted β= -3.98, 95%CI: -5.41, -2.55) and lower SRP (adjusted β= -2.58, 95%CI= -4.79, -0.37). Thematic analyses revealed: (1) contexts of TS, including survival needs and pandemic impacts; (2) intersectional HIV vulnerabilities; (3) reduced HIV prevention/care access; and (4) water insecurity as a co-occurring socio-economic stressor. Multi-method findings reveal FI and WI are linked with HIV vulnerabilities, underscoring the need for HIV prevention to address co-occurring resource insecurities with refugee youth.

Similar content being viewed by others
References
Watts N, Amann M, Arnell N, Ayeb-Karlsoon S. The 2019 report of The Lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. The Lancet. 2019;394:1836–78.
Logie C, Toccalino D, Reed AC, Malama K, Newman PA, Weiser S, et al. Exploring linkages between climate change and sexual health: a scoping review protocol. BMJ Open. 2021;11:e054720.
Stanke C, Kerac M, Prudhomme C, Medlock J, Murray V. Health effects of drought: a systematic review of the evidence. PLoS Curr. 2013;5.
UNICEF, World Food Programme (WFP), World Health Organization (WHO). The State of Food Security and Nutrition in the World 2020. IFAD, UNICEF, WFP and WHO. Italy: FAO; 2020.
UN (United Nations) Water. Sustainable Development Goal 6, Synthesis Report 2018 on Water and Sanitation. Executive summary. Geneva, Switzerland: United Nations; 2018.
Lieber M, Chin-Hong P, Whittle HJ, Hogg R, Weiser SD. The synergistic relationship between Climate Change and the HIV/AIDS epidemic: a conceptual Framework. AIDS Behav. 2021;25:2266–77.
Burke M, Gong E, Jones K. Income shocks and HIV in Africa. Econ J. 2015;125.
Orievulu KS, Ayeb-Karlsson S, Ngema S, Baisley K. Exploring linkages between drought and HIV treatment adherence in Africa: a systematic review. The Lancet Planetary Health. 2022;6:e359–70.
Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94:1729S–39.
Wutich A, Brewis A. Food, water, and scarcity: toward a broader anthropology of resource insecurity. Curr Anthropol. 2014;55:444–68.
Moorhouse L, Schaefer R, Thomas R, Nyamukapa C, Skovdal M, Hallett TB, et al. Application of the HIV prevention cascade to identify, develop and evaluate interventions to improve use of prevention methods: examples from a study in east Zimbabwe. J Int AIDS Soc. 2019;22:86–92.
Kuchukhidze S, Panagiotoglou D, Boily M-C, Diabaté S, Eaton JW, Mbofana F, et al. The effects of intimate partner violence on women’s risk of HIV acquisition and engagement in the HIV treatment and care cascade: a pooled analysis of nationally representative surveys in sub-saharan Africa. Lancet HIV. 2023;10:e107–17.
van Daalen KR, Kallesøe SS, Davey F, Dada S, Jung L, Singh L, et al. Extreme events and gender-based Violence: a mixed-methods systematic review. Lancet Planet Health. 2022;6:e504–23.
Tallman P, Collins S, Salmon-Mulanovich G, Rusyidi B. Water insecurity and gender-based violence: A global review of the evidence. WIREs Water. 2023;10(1):e1619.
Hatcher AM, Page S, Van Aletta L, Pearson I, Fielding-Miller R, Mazars C et al. Systematic review of food insecurity and violence against women and girls: Mixed methods findings from low- and middle-income settings. PLOS Glob Public Health. 2022;2:e0000479.
Low A, Frederix K, McCracken S, Manyau S, Elizabeth G. Association between severe drought and HIV prevention and care behaviors in Lesotho: a population-based survey 2016–2017. PLoS Medicine. 2019;16(1): e1002727.
Pandipati S, Abel D. Anticipated impacts of climate change on women’s health: a background primer. Int J Gynecol Obstet. 2023;160:394–9.
WFP. Global Report on Food Crises – 2022 [Internet]. Rome, Italy: World Food Programme; 2022. Available from: https://www.wfp.org/publications/global-report-food-crises-2022.
Owen M, Kruczkiewicz A, Van Den Hoek J. Indexing climatic and environmental exposure of refugee camps with a case study in East Africa. Sci Rep. 2023;13:7533.
UNHCR. Global Trends Forced Displacement in 2021 [Internet]. Geneva, Switzerland: UNHCR; 2021. Available from: https://www.unhcr.org/publications/brochures/62a9d1494/global-trends-report-2021.html.
Integrated Food Security Phase Classification. IPC Acute Food insecurity Analysis. Rome, Italy: FAO; 2022.
UNHCR. Uganda - Refugee statistics March 2023. Geneva, Switzerland: UNHCR (The UN Refugee Agency); 2023.
World Bank Group. Climate Risk Country Profile: Uganda [Internet]: Climate Change Knowledge Portal. Washington, DC, USA: World Bank Group. 2021. Available from: https://climateknowledgeportal.worldbank.org/sites/default/files/2021-05/15464-WB_Uganda%20Country%20Profile-WEB%20%281%29.pdf.
Kogan F, Guo W, Yang W. Drought and food security prediction from NOAA new generation of operational satellites. Geomat Nat Hazards Risk. 2019;10:651–66.
Sabila S, Silver I. Cities as partners: the case of Kampala. Forced Migr Rev. 2020;63:41–3.
Weiser S, Palar K, Frongillo E, Tsai A, Kumbakumba E, dePee S, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28:115–20.
Tsai A, Bangsberg D, Emenyonu N, Senkung J, Martin J, Weiser S. The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med. 2011;73:1717–24.
Weiser S, Tuller D, Frongillo E, Senkung J, Mukiibi N, Bangsberg D. Food Insecurity as a Barrier to Sustained Antiretroviral Therapy Adherence in Uganda. PLoS ONE. 2010; 5(4): e103402010.
Logie C, Okimi M, Mwima S, Hakiza R, Abela H, Kyambadde P. Gender, transactional sex, and HIV prevention cascade engagement among urban refugee and displaced adolescents and youth in Kampala. Uganda. AIDS Care. 2021;33:897–903.
Logie CH, Okumu M, Mwima S, Hakiza R, Irungi KP, Kyambadde P, et al. Social ecological factors associated with experiencing violence among urban refugee and displaced adolescent girls and young women in informal settlements in Kampala, Uganda: a cross-sectional study. Confl Health. 2019;13:60.
Horn R, Puffer ES, Roesch E, Lehmann H. Women’s perceptions of effects of war on intimate partner violence and gender roles in two post-conflict west African countries: consequences and unexpected opportunities. Confl Health. 2014;8:12.
Mootz JJ, Stark L, Meyer E, Asghar K, Roa AH, Potts A, et al. Examining intersections between violence against women and violence against children: perspectives of adolescents and adults in displaced Colombian communities. Confl Health. 2019;13:25.
Logie CH, Daniel C, Ahmed U, Lash R. ‘Life under the tent is not safe, especially for young women’: understanding intersectional violence among internally displaced youth in Leogane, Haiti. Glob Health Action. 2017; 10(sup2): 1270816
Logie C, Okumu M, Coelho M, Loutet M, Narasimhan M, Lukone SO, et al. Water insecurity and sexual and gender-based violence among refugee youth: qualitative insights from a humanitarian setting in Uganda. J Water Sanit Hyg Dev. 2022;12:883–93.
Logie CH, Okumu M, Loutet M, Berry I, Taing L, Lukone SO et al. Associations between water insecurity and depression among refugee adolescents and youth in a humanitarian context in Uganda: cross-sectional survey findings. Int Health. 2022;1–3.
Hamill MM, Hu F, Adebajo S, Kokogho A, Tiamiyu AB, Parker ZF, et al. Food and water insecurity in sexual and gender minority groups living with HIV in Lagos, Nigeria. JAIDS J Acquir Immune Defic Syndr. 2023;93:171–80.
Logie CH, Okumu M, Mwima SP, Kyambadde P, Hakiza R, Kibathi IP, et al. Exploring associations between adolescent sexual and reproductive health stigma and HIV testing awareness and uptake among urban refugee and displaced youth in Kampala, Uganda. Sex Reprod Health Matters. 2019;27:86–106.
Amara, A.H., Aljunid, S.M. Noncommunicable diseases among urban refugees and asylum-seekers in developing countries: a neglected health care need. Global Health 10, 24 (2014).
Women’s Refugee Commission. The Living Ain’ t Easy Urban Refugees in Kampala. New York, USA: Women’s Refugee Commission; 2011.
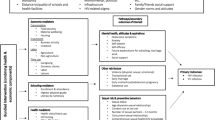
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:1–1.
UNAIDS. Young people and HIV. Geneva, Switzerland: UNAIDS; 2021.
Okeke SR, Idriss-Wheeler D, Yaya S. Adolescent pregnancy in the time of COVID-19: what are the implications for sexual and reproductive health and rights globally? Reprod Health. 2022;19:207, s12978-022-01505–8.
Chimbindi N, Ngema U, Ngwenya N, Gibbs A, Groenewald C, Harling G, et al. The sexual and reproductive health needs of school-going young people in the context of COVID-19 in rural KwaZulu-Natal, South Africa. Afr J AIDS Res. 2022;21:162–70.
Dorward J, Khubone T, Gate K, Ngobese H, Sookrajh Y, Mkhize S et al. The impact of the COVID-19 lockdown on HIV care in 65 South African primary care clinics: an interrupted time series analysis. Lancet HIV. 2021;8.
Decker MR, Bevilacqua K, Wood SN, Ngare GW, Thiongo M, Byrne ME, et al. Gender-based violence during COVID-19 among adolescent girls and young women in Nairobi, Kenya: a mixed-methods prospective study over 18 months. BMJ Glob Health. 2022;7:e007807.
Estlein R, Gewirtz-Meydan A, Opuda E. Love in the time of COVID‐19: a systematic mapping review of empirical research on romantic relationships one year into the COVID‐19 pandemic. Fam Process. 2022;61:1208–28.
Closson K, Ndungu J, Beksinska M, Ogilvie G, Dietrich JJ, Gadermann A, et al. Gender, Power, and Health: measuring and assessing sexual relationship power equity among young Sub-saharan African women and men, a systematic review. Trauma Violence Abuse. 2022;23:920–37.
Closson K, Dietrich JJ, Beksinska M, Gibbs A, Hornschuh S, Smith T, et al. Measuring sexual relationship power equity among young women and young men South Africa: implications for gender-transformative programming. PLoS ONE. 2019;14:1–19.
Adeniyi OV, Ajayi AI, Moyaki MG, Goon DT, Avramovic G, Lambert J. High rate of unplanned pregnancy in the context of integrated family planning and HIV care services in South Africa. BMC Health Serv Res. 2018;18:140.
Kons K, Biney AAE, Sznajder K. Factors Associated with adolescent pregnancy in Sub-saharan Africa during the COVID-19 pandemic: a review of socioeconomic influences and essential interventions. Int J Sex Health. 2022;34:386–96.
Logie CH, Okumu M, Berry I, Hakiza R, Kibuuka Musoke D, Kyambadde P et al. Kukaa Salama (staying safe): study protocol for a pre/post-trial of an interactive mHealth intervention for increasing COVID-19 prevention practices with urban refugee youth in Kampala, Uganda. BMJ Open. 2021;11.
Logie CH, Mobile Health-Supported HIV. Self-Testing Strategy among Urban Refugee and Displaced Youth in Kampala, Uganda: protocol for a Cluster Randomized Trial (Tushirikiane, supporting each other). 7. JMIR Res Protoc. 2021;4504097–7.
Pulerwitz J, Gortmaker SL, Dejong W. Measuring sexual relationship power in HIV/STD Research. Sex Roles. 42:2000.
Brafford LJ, Beck KH. Development and validation of a Condom Self-Efficacy Scale for College Students. J Am Coll Health. 1991;39:219–25.
Logie C, Berry I, Okumu M, Loutet M, McNamee C, Hakiza R, et al. The prevalence and correlates of depression before and after the COVID-19 pandemic declaration among urban refugee adolescents and youth in informal settlements in Kampala. Uganda: A longitudinal cohort study. Annals of Epidemiology. 2020, 66: 37-43.
Logie CH, Lys CL, Sokolovic N, Mackay KI, Donkers H, Kanbari A et al. Contextual factors associated with depression among Northern and indigenous adolescents in the Northwest Territories, Canada. Glob Ment Health. 2021;8.
Dedoose. Web application for managing, analyzing, and presenting qualitative and mixed method research data. 2016.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1:385–405.
Weiser SD, Sheira LA, Palar K, Kushel M, Wilson TE, Adedimeji A et al. Mechanisms from Food Insecurity to worse HIV Treatment outcomes in US women living with HIV. AIDS Patient Care and STDs. 2020;34:425–35.
Logie CH, Sokolovic N, Kazemi M, Islam S, Frank P, Gormley R et al. Does resource insecurity drive HIV-related stigma? Associations between food and housing insecurity with HIV-related stigma in cohort of women living with HIV in Canada. Journal of the International AIDS Society (JIAS). 2022;25:11–4.
Leddy AM, Zakaras JM, Shieh J, Conroy AA, Ofotokun I, Tien PC, et al. Intersections of food insecurity, violence, poor mental health and substance use among US women living with and at risk for HIV: evidence of a syndemic in need of attention. PLoS ONE. 2021;16:1–19.
Low AJ, Frederix K, McCracken S, Manyau S, Gummerson E, Radin E et al. Association between severe drought and HIV prevention and care behaviors in Lesotho: a population-based survey 2016–2017. PLoS Med. 2019;16.
Epstein A, Nagata JM, Ganson KT, Nash D, Saberi P, Tsai AC et al. Drought, HIV Testing, and HIV Transmission Risk Behaviors: A Population-Based Study in 10 High HIV Prevalence Countries in Sub-Saharan Africa. AIDS Behav. 2023; 27(3):855-863.
Orievulu KS, Ayeb-Karlsson S, Ngema S, Baisley K, Tanser F, Ngwenya N, et al. Exploring linkages between drought and HIV treatment adherence in Africa: a systematic review. Lancet Planet Health. 2022;6:e359–70.
Creswell JW. Research Design: Qualitative, quantitative, and mixed methods approaches, 4th Edition. London, UK: Sage Publications, Inc. 2013.
McCrudden MT, Marchand G, Schutz PA. Joint displays for mixed methods research in psychology. Methods Psychol. 2021;5:100067.
Flicker S, Guta A. Ethical approaches to adolescent participation in sexual Health Research. J Adolesc Health. 2008;42.
Malama K, Logie CH, Okumu M, Hakiza R, Mwima S, Kyambadde P. Factors associated with motherhood among urban refugee adolescent girls and young women in informal settlements in Kampala, Uganda. Women Health. 2023;63:51–8.
Groves AK, Gebrekristos LT, Smith PD, Stoebenau K, Stoner MC, Ameyan W, et al. Adolescent mothers in Eastern and Southern Africa: an overlooked and uniquely vulnerable subpopulation in the fight against HIV. J Adolesc Health. 2022;70:895–901.
Christofides NJ, Jewkes RK, Dunkle KL, Nduna M, Shai NJ, Sterk C. Early adolescent pregnancy increases risk of incident HIV Infection in the eastern cape, South Africa: a longitudinal study. J Int AIDS Soc. 2014;17.
Namukisa M, Kamacooko O, Lunkuse JF, Ruzagira E, Price MA, Mayanja Y. Incidence of unintended pregnancy and associated factors among adolescent girls and young women at risk of HIV Infection in Kampala, Uganda. Front Reprod Health. 2023;5:1089104.
Boateng GO, Workman CL, Miller JD, Onono M, Neilands TB, Young SL. The syndemic effects of food insecurity, water insecurity, and HIV on depressive symptomatology among Kenyan women. Soc Sci Med. 2022;295.
Maxfield A. Testing the theoretical similarities between food and water insecurity: buffering hypothesis and effects on mental wellbeing. Soc Sci Med. 2020;244:112412–2.
Uwishema O, Taylor C, Lawal L, Hamiidah N, Robert I, Nasir A et al. The syndemic burden of HIV/AIDS in Africa amidst the COVID-19 pandemic. Immun Inflamm Dis. 2021;1–7.
Arsenault C, Gage A, Kim MK, Kapoor NR, Akweongo P, Amponsah F, et al. COVID-19 and resilience of healthcare systems in ten countries. Nat Med. 2022;28:1314–24.
Funding
This study is funded by the Canadian Institutes of Health Research (Project Grant 389142), International Development Research Centre (IDRC) Operating Grant (109549-001), and Grand Challenges Canada Global Mental Health Grant (R-GMH-POC-2107-43740). Logie’s efforts were in part supported by the Canada Research Chairs Program (CRC 2 in Global Health Equity and Social Justice with Marginalized Populations) and the Canada Foundation for Innovation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
We received Research Ethics Board approval from the University of Toronto (Protocol Number: 37496), Mildmay Uganda Research Ethics Committee (Ref: 0806–2019), and Uganda National Council for Science & Technology (Ref: HS2716). We obtained written informed consent from all participants where data collection was in-person, and verbal informed consent in cases of phone-based data collection. The Tushirikiane trial is registered at ClinicalTrials.gov (NCT04504097).
Conflict of Interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Logie, C.H., Okumu, M., Admassu, Z. et al. HIV Vulnerabilities Associated with Water Insecurity, Food Insecurity, and Other COVID-19 Impacts Among Urban Refugee Youth in Kampala, Uganda: Multi-method Findings. AIDS Behav 28, 507–523 (2024). https://doi.org/10.1007/s10461-023-04240-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04240-8