Measles outbreak propagated by visiting a health facility, in a refugee hosting community, Kiryandongo District, Western Uganda, August 2022 – May 2023
Authors: Saudah Namubiru Kizito1*, Brenda Simbwa1, Kiggundu Thomas1, Richard Akuguzibwe2, Imam Sembatya2, Edrisa Nsubuga1, Daniel Kadobera1, Richard Migisha1, Alex Riolexus Ario1 Institutional affiliations:1Uganda Public Health Fellowship Program, National Institute of Public Health, Kampala, Uganda, 2Kiryandongo District Local Government, Kiryandongo, Uganda, 3Department of National Health Laboratory and Diagnostic Services, Ministry of Health, Kampala, Uganda; *Correspondence: Tel: +256704518351, Email: saudahnam@gmail.com,
Summary
Introduction: Measles outbreaks in refugee settlements are a public health concern due to the potential for rapid spread. Kiryandongo District, Uganda, has a large population of refugees and has experienced measles outbreaks previously due to low vaccination coverage. In December 2022, Kiryandongo District reported an outbreak of measles in the refugee hosting community. We investigated the outbreak to determine its scope, identify risk factors for transmission, evaluate vaccination coverage and effectiveness, identify the barriers and facilitators of vaccination coverage, and recommend evidence-based control measures to prevent future outbreaks.
Methods: We defined a probable case as onset of fever (≥3 days) and generalized rash, plus ≥1 of the following: conjunctivitis, cough, and/or runny nose in a Kiryandongo District resident August-May, 2023. A confirmed case was a probable case with measles-specific IgM (+) not explained by vaccination. We reviewed medical records and conducted active community case-finding. In a case-control investigation involving probable case-patients and controls matched by age and village, we evaluated risk factors for transmission for both cases and controls during the case-patients’s likely exposure period (i.e., 7–21 days prior to rash onset). We estimated vaccine effectiveness (VE) using the formula: VE≈(1-ORprotective) × 100. We calculated vaccination coverage using the percentage of controls vaccinated. We further assessed the factors leading to the low vaccine coverage.
Results: We identified 280 probable cases during the outbreak period (attack rate [AR]=8.2/10,000), including 11 confirmed. Refugees were 73% (205/280) of the total case persons identified in the outbreak. Children aged <1 year were the most affected (AR=70/10,000). Thirty-eight percent of case-patients and 16% of control persons visited a health facility (by themselves or with parents) during the case-patient’s likely exposure period (ORM-H=6.6; 95% CI =2.1-21). Among children aged 3–240 months, the effectiveness of the measles vaccine was 91% (95% CI = 64–98); vaccination coverage was 68% (95% CI = 61–76). Low coverage was due to refugees’ ongoing mobility and the language barrier.
Conclusion: Early case detection and proper health facility isolation of case-patients in addition to strengthening immunization services in refugee settlements is critical to improving vaccine coverage and preventing future outbreaks.
Background
Measles is a highly contagious viral respiratory infection caused by a morbillivirus of the Paramyxoviridae family [1]. It remains a major public health concern globally, despite the availability of an effective vaccine [2]. Refugees and internally displaced individuals are at a heightened risk of experiencing outbreaks of vaccine preventable diseases like measles [3]. Measles outbreaks have been observed in various refugee communities across the globe, driven by factors including poor living conditions, limited healthcare access, insufficient vaccination rates[4, 5]. For example, in Rohingya refugee camps in Bangladesh, the combination of overcrowding and healthcare constraints amplified the measles outbreaks[6, 7]. Additionally, multiple Sub-Saharan African countries have grappled with measles outbreaks, frequently tied to poverty, conflict, and displacement, leading to low vaccination coverage and inadequate healthcare availability [8]. To address these challenges effectively, comprehensive vaccination strategies, enhanced surveillance systems, and strengthened healthcare infrastructure are essential for mitigating the impact of measles outbreaks among displaced populations [9].
Uganda has made significant progress in reducing the burden of measles through the national immunization program [10]. However, measles outbreaks continue to occur in pockets of low vaccination coverage, particularly in refugee camps. In 2019, Uganda reported 9,774 cases of measles, with 7,119 cases occurring in refugee settlements.
Kiryandongo District has a high population of refugees, with over 100,000 refugees from South Sudan and the Democratic Republic of Congo [11]. Vaccination coverage in refugee camps is often below the threshold due to factors such as inadequate healthcare infrastructure, vaccine hesitancy, and mistrust of healthcare providers [12]
At the end of December 2022, a measles outbreak was confirmed in Kiryandongo and Palabek refugee settlements. A cumulative total of 11 confirmed cases by measles IgM were reported from January to February 2023. On 8th February 2023, the Uganda Ministry of Health was notified about the measles outbreak in Kiryandongo District through the Public Health Emergency Operations Centre (PHEOC). We investigated the outbreak to determine its scope, identify risk factors for transmission, evaluate vaccination coverage and effectiveness, identify the barriers and facilitators of vaccination coverage, and recommend evidence-based control and prevention measures.
Methods
Outbreak setting
Kiryandongo is a peri urban district located in western Uganda along the Kampala-Gulu
highway. It comprises of 8 sub-counties and 2 town councils[13] with an estimated population of 287,200 people by 2021.[14] [9]. It was among the first districts to receive and resettle refugees since the onset of the civil conflict in South Sudan. A total of 52,545 individuals were resettled in this refugee and Internally Displaced Persons camp during December 2013-March 2017. Of the total camp population, approximately 99% are from South Sudan, with <0.5% each from Democratic Republic of Congo, Kenya, Sudan, and Uganda. According to UNHCR statistics, 2018 42% of the refugees and internally displaced persons (IDPs) are <18 years of age[15]. The refugee settlement is served by three Health Centre IIs, two Health Centre IIIs, and one General Hospital[14].
The camp exceeded its population and therefore no longer admits new refugees. However, given the free entry and exit nature of the camp, refugees continue to move out and/or receive visitors from the neighboring far and near settlements or move to South Sudan. Like the rest of the country, Kiryandongo participated in the 2022 mass measles campaign. The campaign was conducted in April and October, 2022. While the rest of the district vaccination coverage was 76%, the refuge settlement coverage was 58% in the October campaign.
Case definition and finding
We defined a probable case as onset of fever and generalized rash with at least one of the following symptoms: coryza, conjunctivitis, or cough, in a resident of Kiryandongo District between August 2022 and May 2023. A confirmed case was a probable case with measles IgM (+) in the absence of vaccination in the preceding 2 weeks. We actively searched for case-persons in the community with the help of community leaders, community health workers and EPI (Expanded Program for Immunization) focal persons in the district (i.e., a cadre of public health workers involved in monitoring immunization activities ref). We reviewed surveillance data from the District Health Information System 2 (DHIS2) to identify areas or sub counties affected by the outbreak. We further reviewed health facility records at all health centres that had reported measles cases in the district to update the line list. We conducted community active case search and updated the linelist. Using a standardized case investigation form, we collected data on case-patient’s demographics, clinical information, and exposure history.
Descriptive epidemiology
We assessed the time distribution of measles cases by constructing epidemic curves. We calculated attack rates by age, sex, nationality, subcounty using Kiryandongo District population by extrapolating from the 2014 Uganda National Population Census using the district-specific population growth rates [10]. We presented attack rates by sub-county using a chloropleth map.
Laboratory investigations
Laboratory confirmation was conducted at the Expanded Program for Immunization Laboratory (EPI Lab) at Uganda Virus Research Institute, using the recommended World Health Organization (WHO) procedures[16].
Hypothesis generation
We conducted 20 hypothesis generating interviews amongst case-patients or caretakers of case-patients in the sub-county with the highest attack rate. We asked about potential risk factors for measles transmission 7 and 21 days prior to symptom onset including: visits to health facilities, community playgrounds, and water-collection points, attendance at schools, and either history of travel to Lamwo District or South Sudan-Palabek county or receipt of visitors from the two places with ongoing measles outbreaks within the outbreak period.
Case-control investigation
To test the generated hypothesis, we conducted a matched case-control study in the most affected sub-county. We matched in by village and age in a ratio of 1:1. The case- control study was conducted among children aged 3–300 months because all of thecase-patients were in this age group. We administered the questionnaire to case – patients, caregivers/guardians if the case-patient was a minor. For households with more than one case-patient, the first case to develop a rash was selected for interview. We collected data on the following variables: demographic characteristics, travel to an area with ongoing measles outbreak, congregating at health facilities, water collection points, food collection points, and schools, and measles vaccination status and the doses received.We performed logistic regression to assess the risk factors associated with the outbreak.
Vaccination coverage and vaccine effectiveness
We estimated vaccination coverage (VC) using the percent of control-persons vaccinated.
VE ¼ 1−RR Protective ≈ 1−OR Protective
Vaccination status was obtained from child health card or any medical records obtained from the care takers or through interviews (verbal reports with or without immunization cards).
We also obtained the administrative data on the number of doses of measles vaccines administered reported in the DHIS2 for Kiryandongo District August2022-February2023. In estimating the administrative VC, we used the population estimates for Kiryandongo District provided by the Uganda National Population Census report 2016[10].
Qualitative interviews to assess the reasons for the low vaccination coverage, Kiryandongo refugee settlement, August 2022-December 2023
Through key informant interview, we collected data on the reasons for the low vaccination coverage despite the high measles vaccination effectiveness. The key informants included the village health team members/mobilisers for vaccination, camp commandant, EPI focal persons for the district and camp/settlement and the district immunization focal person.
Ethical consideration
We conducted this study in response to a public health emergency and as such was determined to be non-research. The MoH authorized this study and the office of the Center for Global Health, US Center for Diseases Control and Prevention determined that this activity was not human subject research and with its primary intent being for public health practice or disease control. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy. We obtained permission to conduct the investigation from the district health authorities of Kiryandongo. We obtained written informed consent from all the respondents.
Participants were assured that their participation was voluntary and that there would be no negative consequences for declining or withdrawing from the study (none declined or withdrew). Data collected did not contain any individual personal identifiers and information was stored in password-protected computers, which were inaccessible by anyone outside the investigation team.
Results
Descriptive epidemiology
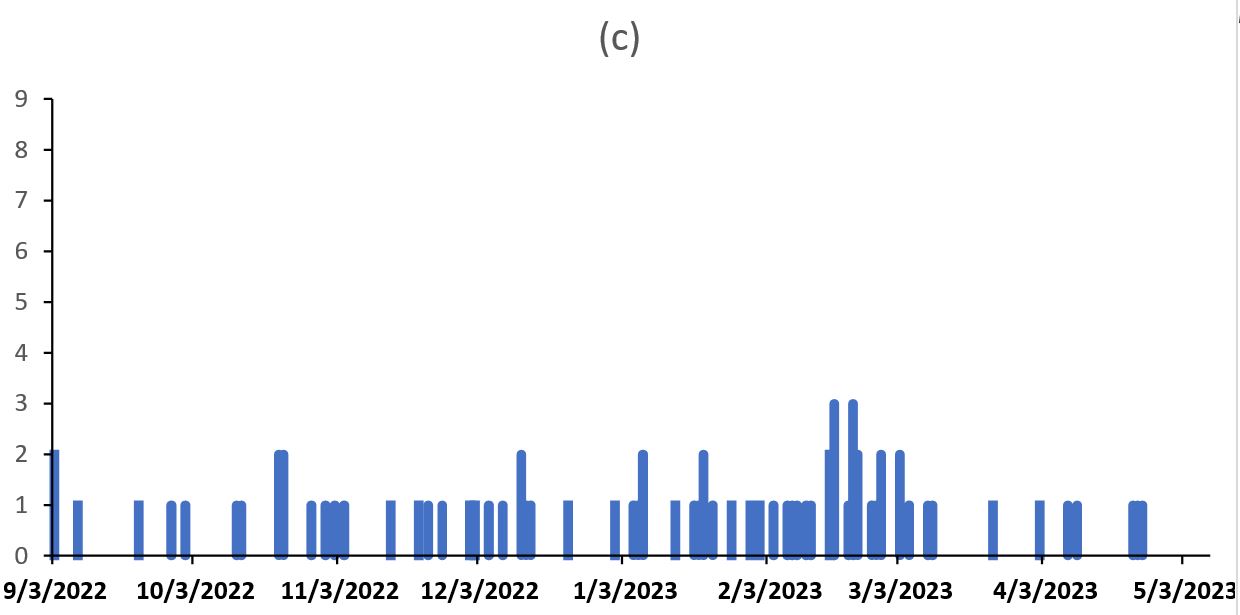
We identified 280 case-patients (overall attack rate [AR] =8.3/10,000), including 11 confirmed by measles-specific IgM. The median age of the case-patients was 35 months (range: 6 months to 45 years). Refugees were 73% (205/280) of the total case- patients identified in the outbreak. The most affected age groups were 0–11 months (AR = 69.5/10,000). Males and females were equally affected. The outbreak affected 5 sub-counties, the most affected being Bweyale Town council (AR = 25.3/10,000) (Figure 1). In Bweyale Town council, the most affected parish was Southern Ward (AR = 33/10,000) followed by Northern Ward (AR = 28/100,000) (Table 1). None of the case- patients exhibited any complications or died.
Table 1: Measles attack rate by age, sex, and sub-county during a measles outbreak: Kiryandongo District, Uganda, August 2022 – May 2023
| Characteristic | Population | Cases | AR/10,000 | |
| Age in years |
Under I year |
13230 |
92 |
69.5 |
|
1-4 |
42943 |
133 |
31 |
|
|
5-9 |
49855 |
30 |
6 |
|
|
≥10 |
116953 |
21 |
1.8 |
|
| Sex |
M |
172,300 |
144 |
8.4 |
|
F |
166,900 |
134 |
8 |
|
| District |
Kiryandongo |
339200 |
280 |
8.3 |
| Parishes in Bweyale TC |
Southern Ward |
63730 |
179 |
28.1 |
|
Northern Ward |
10858 |
36 |
33.2 |
|
|
Central Ward |
16729 |
15 |
9.0 |
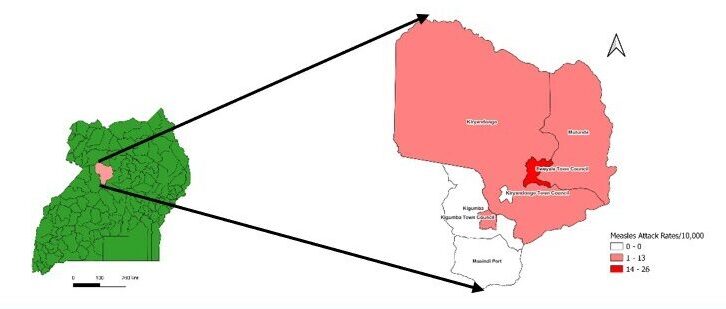
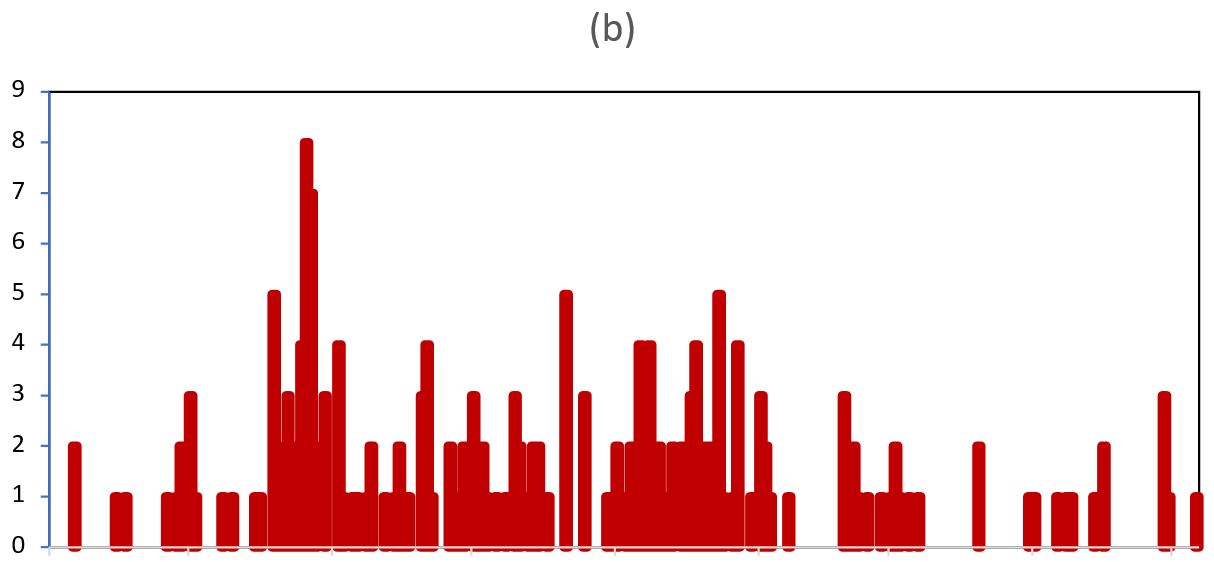
The epidemic curves indicated person-to-person transmission (Figure. 2a). From the symptom onset date of the index case-person (12th August 2022) to that of the last case-person (5th May 2023), the outbreak lasted about 8 months. On 20th August, 2 refugees, reportedly moved from Lamwo district which had been experiencing an outbreak of Measles around that time to visit a relative and a friend in Kiryandongo refugee camp. The district was notified about this travel from Lamwo refugee camp although they couldn’t not trace these refugees. Around the same time, a mother with a 2year old male baby also travelled back from Palabek in South Sudan which also had been experiencing a measles outbreak (where she had gone to check on her husband). A week later, the older siblings and the neighbors also developed similar measles like symptoms. These children were taken to Nyakadoti health centre on September 11th, and samples were taken off. The district was notified about the positive results in November and on 22nd December, the number of cases had increased to include 11 confirmed and hence declared an outbreak. The health facilities continued to receive patients with measles like rash from different parishes and sub-counties.
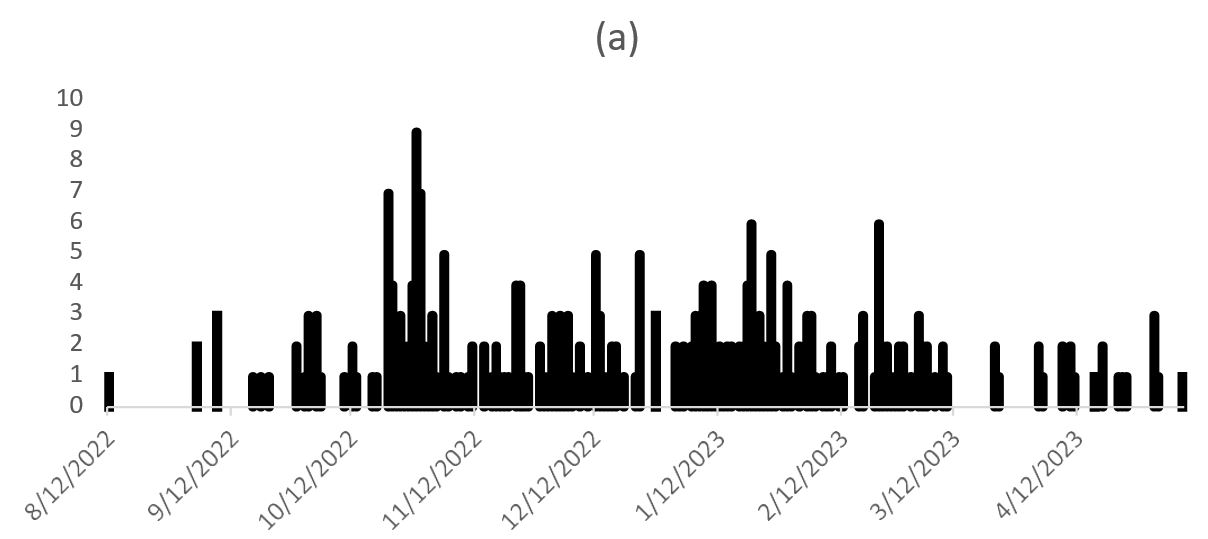
Figure 2: Date of rash onset among measles case-patients August, 2022 – November, 2023. a) district epidemic curve, b) epidemic curve for Refugees, and c) epidemic curve for Nationals |
Hypothesis generation findings
Of the 20 case-patients’/care takers interviewed, 55% attended food collection gatherings for refugees and school, 80% congregated at a health facility, 90% had either travelled to or received visitors from Lamwo or South Sudan while 75% visited a communal water-collection point. We hypothesized that Increased attendance at food collection gatherings, school attendance, congregating at health facilities, and going to communal water-collection points among refugees were associated with a higher risk of measles infection.
Case-control investigation findings
Among persons aged 6–300 months, 56% (56/100) of the case-patients, compared with 26% (26/100) of control-persons, had never been vaccinated against measles during the exposure period ORMH = 0.09 95% CI: 0.02–0.36). Thirty-nine percent (39/100) of the case-patients compared with 14% (14/100) of control-persons, visited a health facility during the exposure period (ORMH = 6.64 95% CI: 2.07–21.23) (Table 2). No other risk factors examined in the case-control investigation was significantly associated with measles onset.
Table 2: Risk factors for measles infection among children aged 3-300months during a measles outbreak, Kiryandongo District, Uganda, August 2022 – February 2023
| Risk factor | % Cases exposed | % Controls exposed | OR MH (95% CI) |
| Vaccinated against Measles | |||
| Yes | 44 | 74 | Ref |
| No | 56 | 26 | 0.09 (0.02-0.36) |
| Visit a Health facility during
exposure period |
|||
| No | 61 | 86 | Ref |
| Yes | 39 | 14 | 6.64 (2.07 – 21.23) |
Measles vaccine effectiveness
From the case-control investigation, 44% (42/100) of case-persons compared to 74% (74/100) of controls had a history of measles vaccination (ORMH =0.09; 95% CI: 0.02-0.36). Using this information, we estimated that VE = 91% (95% CI: 64–98%) in persons aged 6-300months.
Measles vaccine coverage
Of controls aged 6–300 months, 74% (95% CI: 61–76%) had a history of vaccination; this percentage was the estimated VC.
Reasons for the low vaccine coverage for measles vaccine in Kiryandongo Refugee Settlement, February-May 2023
Mobility affects vaccination uptake and coverage
The mobility of families creates barriers to accessing and utilizing vaccination services. Children who are not present in the settlement during vaccination campaigns or scheduled immunization sessions are at risk of missing out on essential vaccinations. “You know this settlement is a free exit and entry. Some families are registered here but live in Bweyale or even Kampala. Some women go (for months) with their small children back to South Sudan to see their husbands. It is hard to get all the children who are due for vaccination ..” (KII interviewee)
Language and Vaccination Participation Challenges
Language barriers between vaccination providers and refugee communities hinder effective communication and engagement, causing reluctance to participate. Limited participation may be due to barriers beyond language.
“…. every year we carry out vaccination campaigns but some people in the refugee communities are still missed because they do not turn up. Even the community sensitization is not helpful because some speak a language that even the VHTs can’t speak,….we cannot ascertain clearly the exact reason for not turning up” (Provider# 9)
Co-ordinating efforts and partnerships
In some instances, providers reported that there were challenges in identifying responder roles and responsibilities and promptly co-ordinating efforts. ‘Perhaps we need to think about [an integrated] model of working with our local
authority partners…. Rather than, “That’s your job. That’s your job,” Where there’s overlap no one’s really doing it, no one’s coordinating it, and then it becomes very much, “You didn’t do this. Why didn’t you do that?” rather than, “How can we make this happen?”’ (Provider#16)
Discussion
The measles outbreak in Kiryandongo refugee settlement from August 2022 to March 2023 was the first measles outbreak following a mass MR vaccination campaign in this area. We investigated the outbreak to determine its scope, identify risk factors for transmission, evaluate vaccination coverage and effectiveness and associated factors. The outbreak was propagated by visiting a health facility whereas low VC and suboptimal VE increased the susceptibility of the population. Two children who travelled from Lamwo refugee settlement which had an ongoing measles outbreak exposed the people.
Congregating at a health facility was associated with increased odds of infection. Other studies have also identified congregation as factors that facilitate the transmission of measles [17, 18].Healthcare facilities are areas where interaction between patients and healthcare workers occurs. If a person at a health facility is sick, there is a high risk that other patients or even healthcare workers, can be put at risk of contracting infection. A similar investigation highlighted that mixing of measles and non-measles patients when they were hospitalized in the pediatric department propagated a measles outbreak in Uganda [17]. In this setting, it is important to educate healthcare workers and patients to recognize possible signs and symptoms of measles, and to appropriately and promptly isolate patients who are experiencing consistent symptoms in order to reduce the risk of propagating measles outbreaks.
The measles coverage in Kiryandongo was estimated at 54% in the settlement while in the host communities it was 62%. Both coverages are lower than the recommended vaccination coverage of > 90% required for herd immunity and for achieving the measles elimination goal set by the WHO for the African Region and adopted by the Uganda Ministry of Health to achieve population immunity [20]. The main reasons for this low vaccination coverage were increased mobility of the refugee population, language barrier, and poorly coordinated immunization efforts and partnerships. A study by Ekezie etal described factors such as poor immunisation rates in refugees’ countries of origin, cultural, religious and personal beliefs and healthcare system barriers as contributory to low vaccination coverage in disadvantaged, isolated, and difficult to reach communities like refugee communities [5].
Study limitations
The study used controls that could be have had asymptomatic infections or in their incubation period of disease likely leading to an under estimation of the true burden of disease among controls.
Conclusion
Early case detection and proper health facility isolation of case-patients in addition to strengthening immunization services in refugee settlements is critical to improving vaccine coverage and preventing future outbreaks.
Conflict of Interest
The authors declare that they had no conflict of interest.
Authors contribution
SKN: participated in the conception, design, analysis, interpretation of the study and wrote the draft bulletin; BS, AR, TK, RM, DK, EN, IS reviewed the report, reviewed the drafts of the bulletin for intellectual content and made multiple edits to the draft bulletin; RM, DK, and ARA reviewed the bulletin to ensure intellectual content and scientific integrity.
Acknowledgments
The authors would like to thank Kiryandongo District health office for the technical and administrative support and the management of Kiryandongo refugee camp and settlement for the administrative support rendered during the outbreak.
Copyrights and licensing
All materials in the Uganda Public Health Bulletin is in the public domain and may be used and reprinted without permission; citation as to source; however, is appreciated. Any article can be reprinted or published. If cited as a reprint, it should be referenced in the original form.
References
- Leung, A.K., et al., Measles: a disease often forgotten but not gone. Hong Kong Med J, 2018. 24(5): p. 512-520.
- Hotez, P.J., T. Nuzhath, and B. Colwell, Combating vaccine hesitancy and other 21st century social determinants in the global fight against measles. Current opinion in virology, 2020. 41: p. 1-7.
- Lam, E., A. McCarthy, and M. Brennan, Vaccine-preventable diseases in humanitarian emergencies among refugee and internally-displaced populations. Human vaccines & immunotherapeutics, 11(11): p. 2627-2636.
- Helou, M., G. Van Berlaer, and K. Yammine, Factors influencing the occurrence of infectious disease outbreaks in Lebanon since the Syrian crisis. Pathogens and global health, 116(1): p. 13-21.
- Ekezie, , et al., Access to Vaccination among Disadvantaged, Isolated and Difficult-to-Reach Communities in the WHO European Region: A Systematic Review. Vaccines, 2022. 10(7): p. 1038.
- Chan, E.Y., C.P. Chiu, and G.K. Chan, Medical and health risks associated with communicable diseases of Rohingya refugees in Bangladesh 2017. International Journal of Infectious Diseases, 68: p. 39-43.
- Islam, M.M. and T. Nuzhath, Health risks of Rohingya refugee population in Bangladesh: a call for global Journal of global health, 2018. 8(2).
- Africa, A.o.S.o.S., Root Causes of Low Vaccination Coverage and Under- Immunisation in Sub-Saharan Africa.
- Bile, K., et al., Protecting the right to health of internally displaced mothers and children: the imperative of inter-cluster coordination for translating best practices into effective participatory action.
- Mensah, E.A. and S.O. Gyasi, Measles-Rubella Positivity Rate and Associated Factors in Pre-Mass and Post-Mass Vaccination Periods: Analysis of Uganda Routine Surveillance Laboratory Advances in Public Health, 2022. 2022.
- UNHCR, The Global Accessed on: September 20, 2023. Available from: https://www.unhcr.org/what-we-do/reports-and-publications/global-report. 2022.
- Yazdani, Y., et al., Predictors of COVID-19 Vaccine Acceptability Among Refugees and Other Migrant Populations: A Systematic Scoping Review. medRxiv, 2023: 2023.09. 15.23295608.
- GoU, Kirayndongo District Local Government report,2022. Accessed on September 25th 2022.A vailable from https://www.kiryandongo.go.ug/population.
- Opio, D.N., Evaluation of the Surveillance System in Kiryandongo Refugee Settlement, Kiryandongo District, Uganda, April 2017. J Interval Epidemiol Public Health, 4(4): p. 16.
- Ndegwa, D.G., Contemporary Forced Migration in Africa, in Routledge Handbook of Contemporary African Migration. 2023, Routledge. 182-196.
- Organization, W.H., Manual for the laboratory diagnosis of measles and rubella virus infection. 2007, World Health
- Biribawa, C., et al., Measles outbreak amplified in a pediatric ward: Lyantonde District, Uganda, August BMC infectious diseases, 2020. 20(1): p. 1-8.
- Nsubuga, J., et al., Investigation of a Measles Outbreak in Semuto Subcounty, Nakaseke District, Uganda, June–August 2021.
- Majwala, R.K., et al., Measles outbreak propagated by children congregating at water collection points in Mayuge District, eastern Uganda, July–October, 2016. BMC infectious diseases, 2018. 18: p. 1-7.
- van Boven, M., et al., Estimation of measles vaccine efficacy and critical vaccination coverage in a highly vaccinated population. Journal of the Royal Society Interface, 7(52): p. 1537-1544.